Happy New Year! We recognize that this year is starting on a somber note. We are still witnessing the unfolding holiday surge. As of January 7, we stand at 21.3 million COVID-19 cases in the US, with 361,312 deaths. Some health systems are on the brink of collapse. In LA, over 1,000 people died in less than a week and oxygen is being rationed.
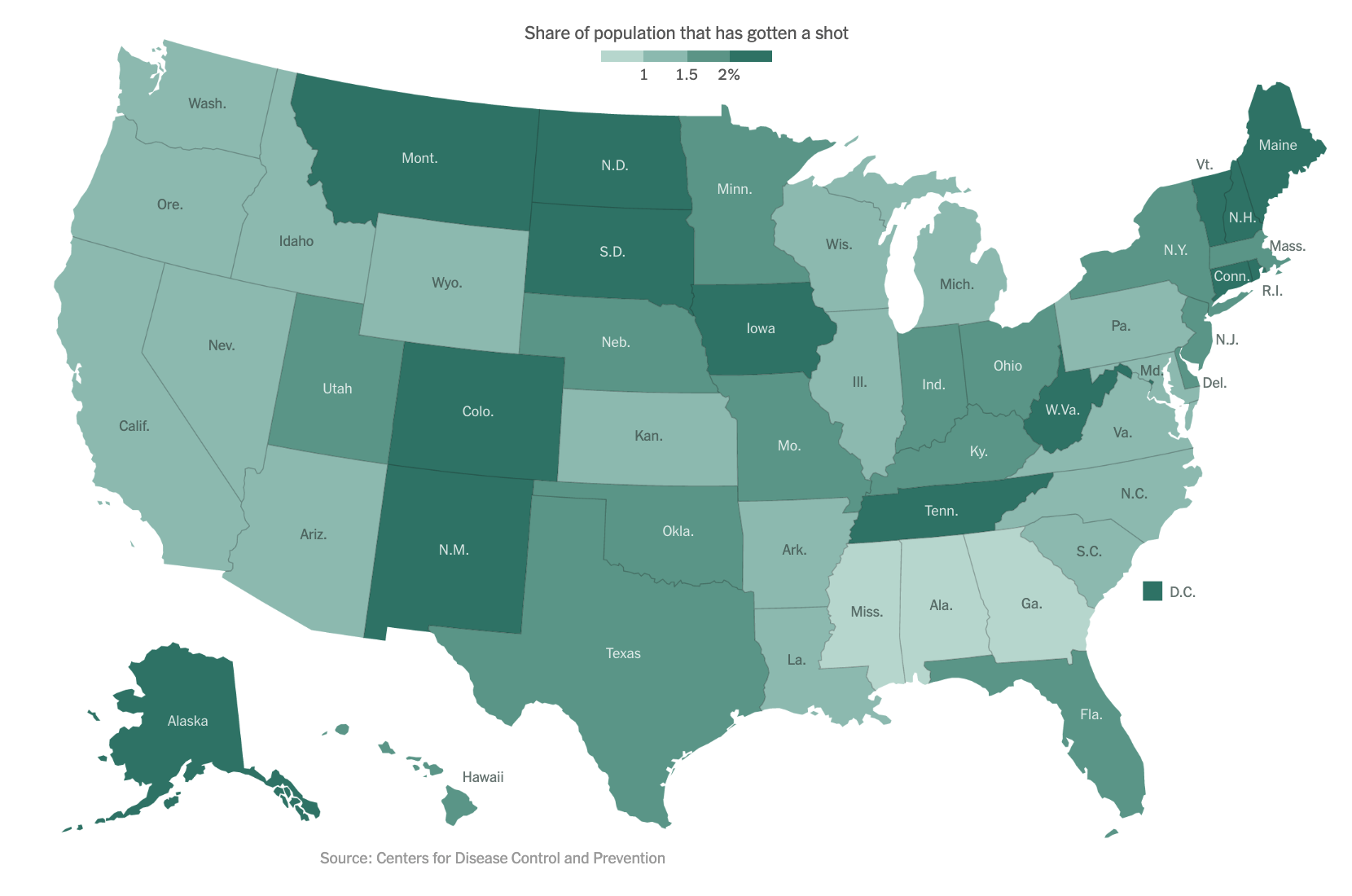
As of our last update on December 14, the Pfizer/BioNTech vaccine had just been granted Emergency Use Authorization (EUA) by the FDA. On December 18, the FDA also granted an EUA to Moderna’s mRNA-based vaccine. As of January 6, approximately 5.3 million people in the US have received at least one vaccine dose, far short of the goal federal officials had set. The below figure shows the percentage of people who have been vaccinated in each state, with light green representing fewer and dark green representing more:
Now that the vaccines are here, many people wonder when they will be eligible to receive one or even if they should get one. By now, you are probably familiar with the concept of the “phased approach” for vaccine roll-out. Initially, there was an effort to vaccinate healthcare workers and other essential workers. Now, there is growing emphasis on vaccinating those over age 75 or with existing co-morbidities.
Prioritization of Patients with Cancer
As patient advocates, we have been actively involved in discussions to urge prioritization of patients with lung cancer for vaccination against COVID-19. During our hiatus from these updates, the COVID Lung Cancer Consortium, convened by Drs. Fred Hirsch, Paul Bunn and John Minna and representing a global assembly of leaders in thoracic oncology, virology, immunology, vaccines, advocacy, as well as the NCI and FDA, wrote a statement urging officials to prioritize ALL patients with cancer, but especially those with lung cancer for vaccination. All of the leading oncology professional societies have also issued similar statements, including ASCO, AACR, ESMO, and SITC.
Vaccine comparison
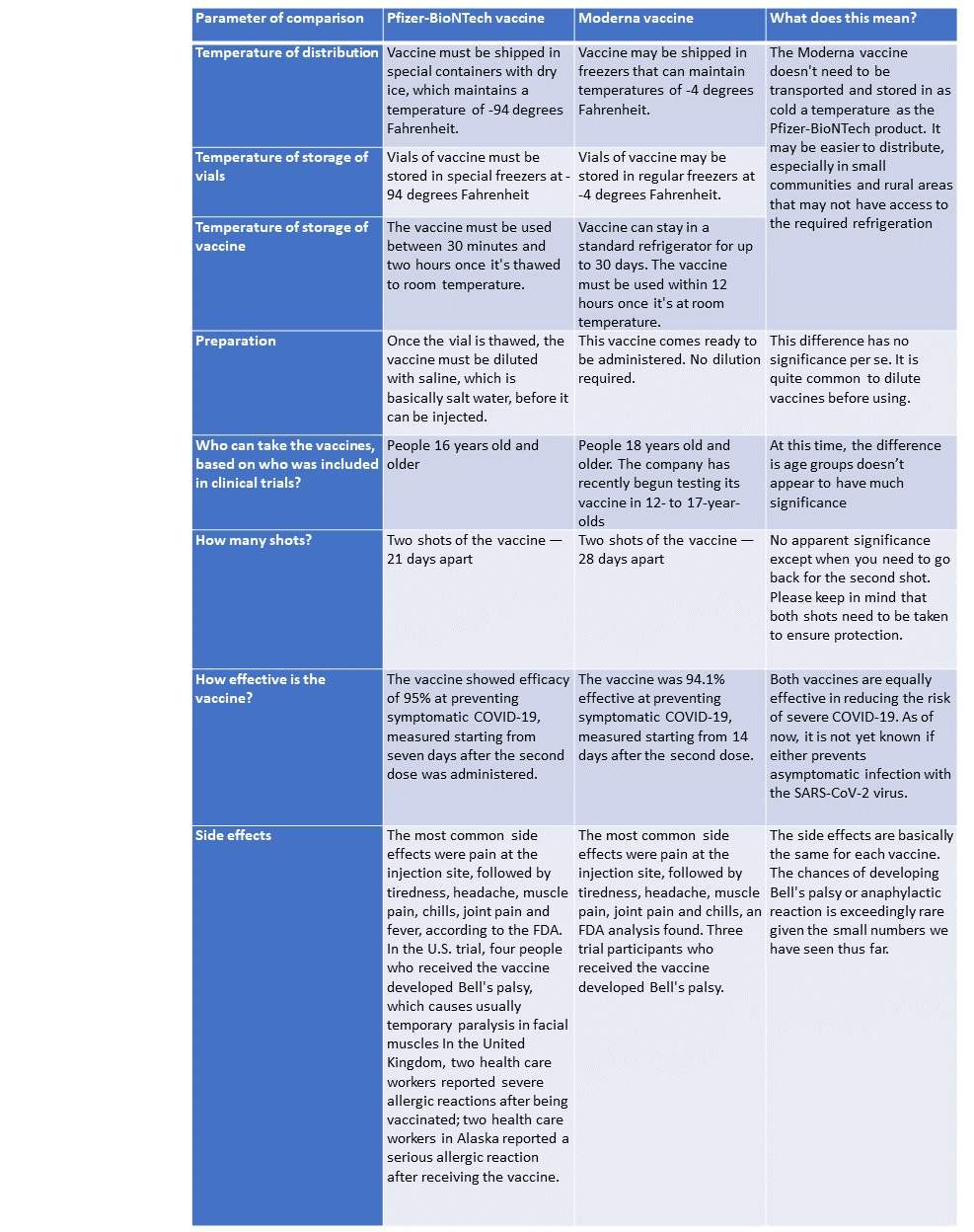
As vaccines become more widely available, , people are asking if one vaccine is better than another. Here we offer a quick comparison of the Pfizer-BioNTech and Moderna vaccines (note, we will not discuss the Oxford/AstraZeneca vaccine as it is not yet approved here in the US). As you can see from the table below, both vaccines are equally effective, and the choice of vaccine may be dependent on the state you live in or what your hospital offers.
New COVID-19 variants
There has been a lot of media attention on new variants of the virus that have been detected in the UK, South Africa and even here in the US. Multiple states are now reporting the presence of the variant first detected in the UK. What does all this mean?
The short answer is we don’t fully know. Different viruses with different “constellations” of mutations are arising independently in different locations around the globe. In the case of the UK variant, it appears to be more transmissible i.e. it can pass more easily from an infected person to a non-infected person. There are concerns that the South African variant may not be as susceptible to current vaccines. BUT, we are awaiting more information.
More studies are needed to confirm the impact of these variants on transmissibility (how easily virus spreads between people), infectivity (how easily it enters the body’s cells), disease severity, immune response and vaccine efficacy. It is still expected that current vaccines will offer some degree of protection against the new variants.
What are the immediate implications for our community?
- We should remain vigilant in practicing public health measures, including wearing masks, washing hands and watching our distance.
- If the variants are more easily transmitted, this could overburden our fragile healthcare system, which is under enormous strain from the holiday surge.
- We must increase our efforts around contact tracing and identifying pockets of these new variants.
- We must rapidly increase vaccination efforts nationwide.
Upcoming events:
January 15: IASLC webinar moderated by Dr. Christian Rolfo on “Managing Clinical and Translational Research During COVID”
January 19: GO2 for Lung Cancer “Lung Cancer Living Room” with Dr. Amy Moore and Dr. Fred Hirsch “New Year, New Era: Ushering in a New Generation of Vaccines”
Resources and websites
- IASLC’s Guide to COVID-19 and Lung Cancer
- The National Cancer Institute website for COVID-19 and emergency preparedness COVID-19: What People with Cancer Should Know
- Updates from the World Health Organization (WHO) and the US Centers for Disease Control and Prevention (CDC)
- Johns Hopkins COVID-19 Resource Center
- Interactive map of US COVID-19 cases by state
- COVID-19 in patients with cancer: managing a pandemic within a pandemic
- You can find information specific to your state or city or town on your health department’s website.
- American Medical Association resources for healthcare providers.

GO2 for Lung Cancer (Amy Moore, PhD – amoore@go2.org)
LUNGevity Foundation (Upal Basu Roy, PhD, MPH – ubasuroy@lungevity.org)
Lung Cancer Foundation of America (Kim Norris – KNorris@lcfamerica.org)
Lung Cancer Research Foundation (Cristina Chin, LMSW, MPH – cchin@lcrf.org)
LungCAN (Kimberly Lester – kimberly@lungcan.org)

I’m SOOOOO GREATFUL FOR AAALLL OF UR HELP AND THE WORK YOU DO AND I’M SO GREATFUL FOR FINDING THIS AND I TRULY TRULY WANT TO THANK YOU AAALLL !!! I’m absolutely sending the information on this foundation to the city and state officials who I know those I don’t know N to the rest of the people I can!!!! I’m proud to be a donor but I wish I could be a REAL donor but I barely scrape on 800$ mthly but I will just do it every single time I can!!!