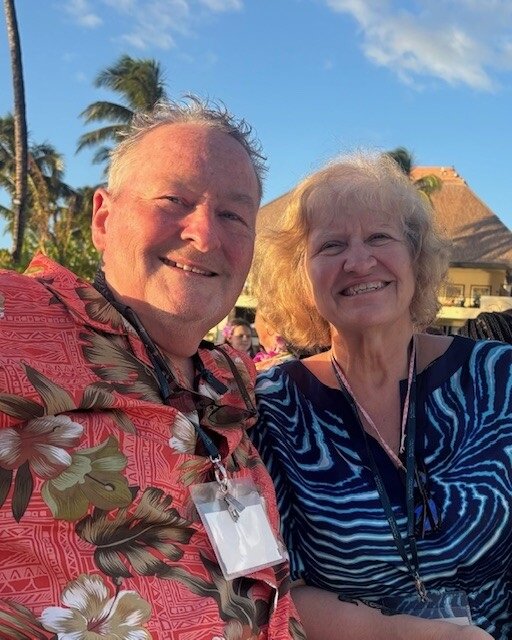
Gary W. and his wife of 44 years reside in Camp Hill, PA—nestled between Gettysburg and Hershey. They credit their children and grandchildren with inspiring them and keeping them young. He’s committed to advocating for the needs of the lung cancer community and helping to ease the uncertainty of those newly diagnosed.
My diagnosis
 My wife has a goal of visiting all 50 states—we’ve been to about 42 so far. We both love National Parks, so at 59 years old, I retired and we booked a trip out west to visit some more. Halfway through that trip, we were unknowingly exposed to COVID. Knowing that people were contagious before they started to show symptoms or test positive, I was aware that we might get sick.
My wife has a goal of visiting all 50 states—we’ve been to about 42 so far. We both love National Parks, so at 59 years old, I retired and we booked a trip out west to visit some more. Halfway through that trip, we were unknowingly exposed to COVID. Knowing that people were contagious before they started to show symptoms or test positive, I was aware that we might get sick.
Sure enough, when we got home, I also came down with COVID. With it, I developed a cough that felt unproductive, like there was something deep in my lungs that I needed to get out but couldn’t. I recovered from COVID and my cough subsided for a little while, but it eventually came back.
I went to my primary care physician who listened to my lungs and told me that he didn’t like the sound of them. He sent me for a scan immediately, where they found a tumor in my lower right lobe. That kicked off a whirlwind of more testing that revealed a tumor in my other lung as well. I was diagnosed with bilateral stage 4 (IV) non-small cell lung cancer with the HER2 mutation.
I had some trouble with my first care team, so I got a second opinion at Johns Hopkins in Washington, D.C. From the very beginning, my oncologist there was very interested in my case and made me feel like he cared about me personally. The HER2 mutation is found in both lung cancer and breast cancer, so he actually put me on a breast cancer drug called Enhertu (fam-trastuzumab deruxtecan-nxki).
Treatment
 I’ve been taking Enhertu (fam-trastuzumab deruxtecan-nxki) for about 2 years now, and I’m doing well on it. My treatments are on Monday mornings. My wife and I usually drive down to my son’s house on the Saturday or Sunday before, spend time with our family, and then go for my infusion on Monday. My treatment begins at 7:15 a.m., and we are usually on our way home by 9:30 a.m. or so.
I’ve been taking Enhertu (fam-trastuzumab deruxtecan-nxki) for about 2 years now, and I’m doing well on it. My treatments are on Monday mornings. My wife and I usually drive down to my son’s house on the Saturday or Sunday before, spend time with our family, and then go for my infusion on Monday. My treatment begins at 7:15 a.m., and we are usually on our way home by 9:30 a.m. or so.
I’ve been blessed that my side effects have been minimal. I’ve been in treatment long enough now that I know that in week 1, I’ll feel pretty run down; in week 2, I’ll start to feel much better; and by week 3, it’s like I don’t even have cancer. I’m able to be very active. I walk with a friend of mine for about 2 miles every day and I also do a lot of our household chores like cooking, cleaning, shopping, and the laundry. In these ways, being in treatment hasn’t changed my day-to-day life too much.
Cancer treatment is incredibly expensive. My wife still works, so I’m on her health insurance. When I first started, my treatments were $32,000 every 3 weeks. The cost has since risen to almost $60,000 per treatment. With my wife’s insurance, we pay only a specialty care visit fee of $40 each time. We are so grateful to have such good coverage. It’s something you don’t think about when you’re diagnosed but it can make a huge difference in how you are able to be treated or whether you can be treated at all.
Approaching lung cancer with a positive attitude
When I was first diagnosed, we were stunned. We truly couldn’t believe it. For several weeks I was in some level of denial about what was going on with me. There was a lot of anxiety, too, because so much is uncertain. You’re always waiting for an appointment, test result, or waiting to see how a treatment will go.
My hair fell out at first, but then it grew back in. I asked my doctor if it was normal to have hair grow back while you’re still in treatment and he said, “There is no such thing as normal here. No 2 people are alike.” That was shocking to me at first, but it also gave me permission to have my own experience with lung cancer and not worry about what happened to other people.
After a little while, you settle into a rhythm and it begins to feel like your regular life. I’m lucky that I’m doing so well on my treatment that I very much live like a normal person. I also made a conscious decision not to be a “Debbie downer” about my diagnosis. There’s no point to it. My quality of life is excellent—what good would it do me to feel sorry for myself about something that’s out of my control? I don’t ever want to stop living and enjoying my life. I was determined not to let lung cancer slow me down…if anything, it’s accelerated me.
One time, I was at the beach in New Jersey with my family and I saw a turtle up near the dunes who was buried in the sand. All you could see was her head sticking out. It may have been a mom who got buried while she was laying her eggs. I watched her work and work to dig herself out of where she’d been buried, and then so very slowly crawl across probably 200 feet of sand to the ocean. It may sound silly but seeing her do that stuck with me. It showed me that we’re all capable of doing hard things if we don’t give up and push forward.
I once had someone ask me, “How many months did they give you?” I said, “I hope a heck of a lot because there’s so much I still want to do before I check out.” The person didn’t know what to say after that, but it’s the truth. I’m not done living. Why would I dwell on anything else but how much I have to be grateful for?
Advice for others living with lung cancer
I will talk to anybody who will listen to educate them about lung cancer. I think the thing that people who are diagnosed with lung cancer really need to understand is that there is so much progress being made with the disease and so much hope. If we’d been diagnosed 8 or 10 years ago, there would have been few options for treating and managing this disease.
When I first met my oncologist, he told me that we have learned more about lung cancer in the past 2 years than in the previous 2 years before that. He told me not to worry because if my treatment ever stops working, or if the side effects get to be too bad to tolerate, he’ll just put me on something else. People need to understand that whatever treatment plan they’re on, it is not the only option. With so much research and new treatments, there may be more therapies and trials in the future. This should bring us all a lot of hope that we can live very well, even with lung cancer.

Very proud of your outlook, Dad! 💕🐢 Thanks for sharing your story!
My husband could sure use some of that positive insight. He is 38 years old recently diagnosed with stage 3c non small cell lung cancer possibly stage 4. ( waiting on test results ) he is allergic to one of his immunotherapies and we are finding it so hard to navigate life and the next steps.
Hi Annie, this is Gary W. I’m sorry you & your husband know too well how challenging this diagnosis can be. I would be honored to do everything I can to help both you & your husband navigate his experience with more certainty & resolve. I certainly don’t have all the answers he might be looking to learn, but I have a few I found that so impacted my journey. Would love to connect if you believe that could ease some anxiety while pending test results are forthcoming. I see the GO2 resource team has reached out too. Please contact them & I’m sure a connection with me (or many other likely more qualified survivors) can be arranged,
Hi Annie, thanks for your comment to Gary’s story. GO2 for Lung Cancer has services, including the Phone Buddy and LungMATCH programs, that may help. If you’d like to learn more, please reach out to us on our HelpLine at 1-800-298-2436 or support@go2.org. We are here to help.
Gary, what a testament to you and your perseverance and to LOVE. Congratulations on this victory. Stay strong. You have people around you who love you very much.