By Shelly Engfer-Triebenbach
 I was just finishing up my 18th year of teaching music when I noticed myself getting short of breath doing easy things. I went to see my primary care doctor who gave me antibiotics and an inhaler so I could treat what they thought was “pneumonia.” I went back the next day because it felt like my breathing had worsened. A pulmonologist ordered a chest X-ray and then sent me to have a heart echocardiogram which confirmed that I had extra fluid around my heart. I had a pericardiocentesis in which 1.5 liters of fluid was drained from what is called the pericardial sac around my heart, and almost immediately I had an easier time breathing and felt better.
I was just finishing up my 18th year of teaching music when I noticed myself getting short of breath doing easy things. I went to see my primary care doctor who gave me antibiotics and an inhaler so I could treat what they thought was “pneumonia.” I went back the next day because it felt like my breathing had worsened. A pulmonologist ordered a chest X-ray and then sent me to have a heart echocardiogram which confirmed that I had extra fluid around my heart. I had a pericardiocentesis in which 1.5 liters of fluid was drained from what is called the pericardial sac around my heart, and almost immediately I had an easier time breathing and felt better.
The next week I had a follow up appointment with a cardiologist. I was told that they found malignant cells (cancer cells) in the fluid from around my heart. I remember praying so hard for breast cancer because I knew the chances of survival were good and that it was a well-researched cancer. Many tests and several days later, I was told I had stage 4 non-small cell lung cancer. I was shocked and in disbelief. How could I have lung cancer? After all, I didn’t smoke!
The value of second opinions and biomarker testing
The tumor was in the upper right lobe of my lung so I had to have a needle-guided biopsy. The tissue was tested for two biomarkers, ALK and EFGR. If my results showed I had one of these biomarkers, I could have targeted therapy instead of chemotherapy. Both came back negative. Devastated, I started chemotherapy the next week, but I was not settled with my diagnosis. I sought out four second opinions. At the fourth, the oncologist wanted to send my initial tissue sample to a company called Foundation One for comprehensive biomarker testing, in case future research identified a biomarker that I did have. When the test came back, we were pleasantly surprised that I had the ALK biomarker after all. I was THRILLED! I felt as though I had won the lung cancer lottery! Being diagnosed ALK+ meant I had the chance to take targeted therapy—giving me more options for my treatment plan.
Learning about my brain metastases
I started on crizotinib after my cancer spread following my first and second lines of treatment. After joining an online patient group, I learned that crizotinib is not effective in the brain, and that I should have a brain MRI at least every six months. I scheduled a brain MRI even though I didn’t have symptoms of the cancer spreading to my brain like dizziness, trouble speaking, or balance issues. During that scan, they discovered that I had seven new spots on my brain.
Finding a path forward with brain metastases
I met with three different radiation oncologists, who all wanted me to have whole brain radiation therapy (WBR). This was in February 2015 and alectinib and brigatinib were both still in clinical trials. After much thought, I joined the brigatinib trial in hopes it would diminish my brain mets and allow me to avoid whole brain radiation. I had twenty-eight glorious months on brigatinib before I had progression to my brain again. This time the brain mets (lung cancer that has spread to the brain) were too numerous to count. My oncologist recommended I travel to Boston to join Dr. Shaw’s clinical trial of lorlatinib.
My first experience with brain radiation
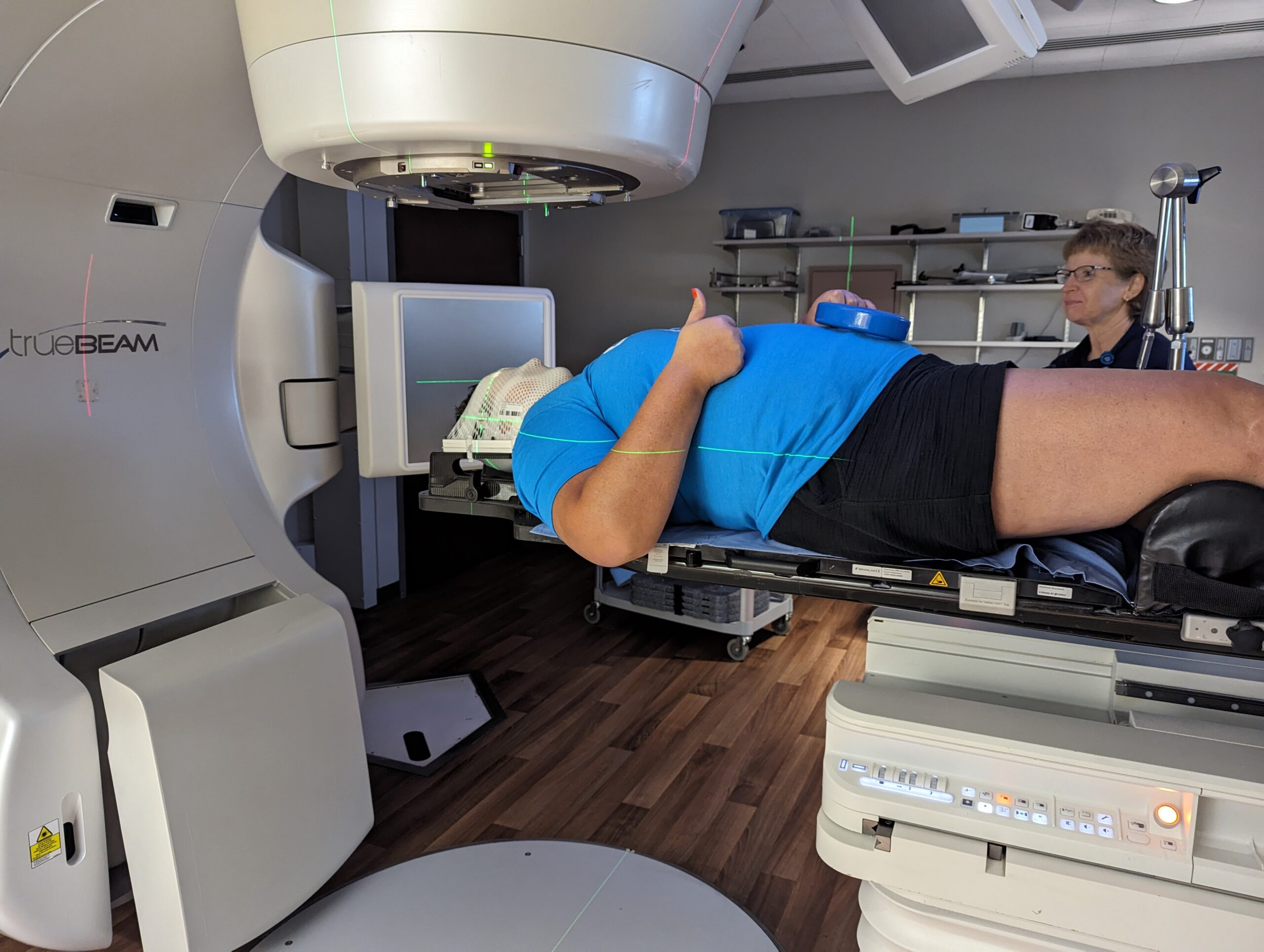
In July 2017, I started on a lorlatinib clinical trial, dodging brain radiation again. In May of 2018, I had mapping and a mold done for stereotactic radiosurgery (SRS). This is a very precisely aimed radiation beam that can treat the one spot on my brain instead of radiating the whole brain. The mold was made from my mouth, as that is how I was attached to the SRS machine. I had one spot in my brain that was not responding to lorlatinib and it was radiated.
SRS was painless. I know it sounds strange, but I didn’t mind being bolted to the machine because everything was very well explained to me by the nurses and doctors. The procedure went according to plan and I felt nothing.
Continued treatment with brain radiation

A year after SRS, the spot that was radiated showed growth. I had surgery in June 2019, followed by ten rounds of focused brain radiation on the growing spot. In preparation, I was fitted with a mask. The mask bolted into the radiation machine to keep me very still.
Each session only lasted about 10 minutes a day. It took longer to change into the gown and get into the machine than it took to do the actual radiation. I was lucky and felt nothing more than a warming sensation and did not have any additional side effects. The treatment was successful, and I did not have any brain mets since the radiation until very recently.
Where I am today
I am lucky that my lung cancer mets continue to be stable in my spine and chest, but last month my care team discovered one on my left optic nerve (a very unusual place) so I needed to have focused brain radiation again. Thankfully I did not have any symptoms, but since it grew so fast, we had to act quickly. I completed five total treatments at the end of June and am continuing to take lorlatinib.
Even though I’m retired from my music teaching career, I volunteer at my local school. I also lead worship music at my church. My lung cancer advocacy work has taken me all over the world and I wouldn’t change one thing. I only wish I was able to do more.
All things considered, I believe I am blessed to be alive ten years after my diagnosis. I have been in two clinical trials and I’m on my sixth line of treatment with high hopes that research will catch up with me and there will be another therapy waiting for me as I need one.
Want to learn more about clinical trials? The GO2 team can provide you or your loved ones with free, one-on-one support. Call our HelpLine at 1-800-298-2436, support@go2.org or submit your question using the form on this page.

[…] post My Experience with Brain Radiation appeared first on GO2 for Lung […]