As different states are relaxing shelter-at-home orders and businesses are planning to re-open, it is important to understand the true extent of COVID-19 infections: both active infections (patients who are currently infected) and past infections (patients who were infected in the past and have now recovered).
Currently, active infections are tested using a nasal swab test. The FDA also recently approved a rapid antigen detection test to identify actively infected cases.
Past infections are identified through serological (blood) tests that detect antibodies against the SARS-CoV-2 virus.
The following infographic shows the differences between the tests used for COVID-19.
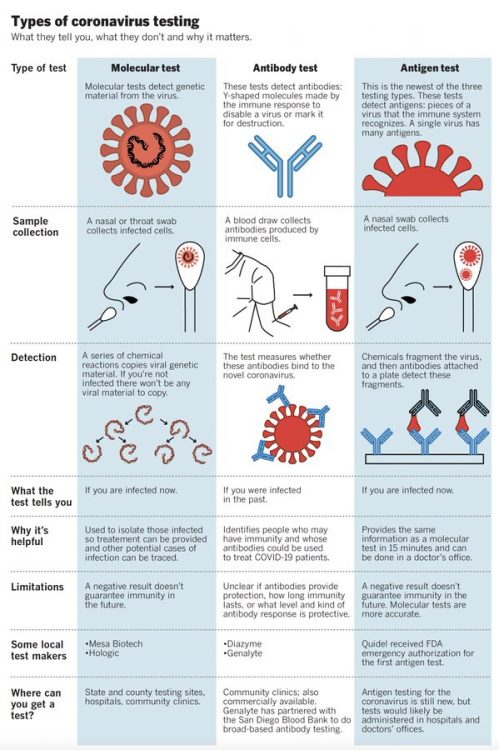
Infographic courtesy: Dr. Jonathan Wosen and Michelle Gilchrist from the San Diego Tribune
However, interpreting the results of the test may be tricky. Also, the results depend on various factors:
- Patient-specific factors: Did the patient mount a robust immune response? How long do detectable antibodies last?
- Test being used: Different antibody tests may have different sensitivity and specificity. We are still learning what this means for different tests and how to interpret the results.
- What an test is measuring: Some tests measure only one type of antibody (IgG) while others measure IgM and IgG. Does this mean one test is better than the other? We still do not know.
- What the test results mean: Does a positive test result mean that a person is immune to re-infection by SARS-CoV-2? If so, for how long?
For example, Amy (in the SF Bay Area) got sick on January 23, 2020 and her antibody test from May 15, 2020 was negative. Upal (in New York City) got sick on March 14, 2020 and his antibody test from May 4, 2020 was positive. Could this be because Amy didn’t produce enough antibodies? Because the antibodies decrease with time? Because the test was not done correctly? Or could it reflect differing test sensitivity?
To answer these types of questions will take time. In case you want to learn more about the issues with interpreting test results, please read the article here.
In this week’s update, we present a short video (and transcript of the discussion) with Dr. Nicolas Vabret, Assistant Professor of Medicine, Hematology and Medical Oncology at Icahn School of Medicine at Mount Sinai. Dr. Vabret, a virologist/immunologist, answers important questions, such as:
- What type of an immune response does the body mount against SARS-CoV-2, the virus that causes COVID-19?
- How can we detect if a person is infected with SARS-CoV-2 now?
- How can we detect if a person was infected with SARS-CoV-2 in the past but has now recovered?
Resources and websites:
- IASLC’s Guide to COVID-19 and Lung Cancer
- The National Cancer Institute has a special website for COVID-19 and emergency preparedness. COVID-19: What People with Cancer Should Know-
- We are following updates provided by the World Health Organization (WHO) and the US Centers for Disease Control and Prevention (CDC)
- Johns Hopkins COVID-19 Resource Center
- Interactive map of US COVID-19 cases by state
- The One-Two Punch: Cancer And COVID-19 (an important perspective for cancer patients)
- You can find information specific to your state or city or town on your health department’s website.
- American Medical Association resources for healthcare providers.



GO2 for Lung Cancer (Amy Moore, PhD – amoore@go2.org)
LUNGevity Foundation (Upal Basu Roy, PhD, MPH – ubasuroy@lungevity.org)
Lung Cancer Foundation of America (Kim Norris – KNorris@lcfamerica.org)
Lung Cancer Research Foundation (Jan Baranski, PhD – jbaranski@lcrf.org)
LungCAN (Kimberly Lester – kimberly@lungcan.org)

Leave A Comment