As of June 28, 2020, the United States has reported more than 2.5 million cases of COVID-19 and 125,484 deaths. We are now seeing a rapid escalation in cases in states across the US. Some would argue that these increases simply reflect more testing but that only tells part of the story. Perhaps a more meaningful metric is the rate of new hospitalizations and ICU bed capacity. Seven states (AZ, AR, CA, NC, SC, TN, TX) are now reporting their highest hospitalization rates since the pandemic started. In hard-hit Houston, TX, ICU bed occupancy stands at 97% at Texas Medical Center. Though only a quarter of that number is currently due to COVID-19 cases, there is once again growing concern about the ability of our hospitals to handle the rapidly increasing number of patients, especially once a second wave of infections strikes.
There are also some changing demographics with this most recent uptick in cases, including growing numbers among young adults ages 20-30. While that may seem to be good news at first, since younger people for the most part have a less severe form of the disease than the elderly or those with underlying comorbidities, this also creates a potential reservoir of the virus that could rapidly extend to more vulnerable populations in the surrounding community.
In the absence of a vaccine or an effective treatment, our best modes of protection remain continued social distancing, frequent handwashing, and wearing masks or facial coverings. This paper from The Lancet supports the use of face masks in reducing transmission in both the healthcare and community setting. The lack of a spike in cases related to recent national protests also suggests that masks played a large role in preventing transmission of the virus. As cases continue to rise across the country, more and more states are beginning to mandate the use of masks or facial coverings, as shown below:

Additional studies on outcomes, antibody response, and radiological findings:
- In our June 15, 2020 update, we presented findings from the TERAVOLT study, which has reported an increased mortality rate (33%) in lung cancer patients with COVID-19. Some have questioned this study’s findings and how translatable they are to the situation here in the US. New data from Memorial Sloan Kettering Cancer Center (MSKCC) in NYC were reported for a cohort of 102 patients with both lung cancer and COVID-19. Of these patients, 62% were hospitalized and 25% died. Of the patients who required ICU level care (21%), 72% died. However, COVID-19 severity appeared to correlate more with patient-specific factors rather than tumor-specific characteristics or treatments. Thus, while this is a small study, it does reinforce the vulnerability of lung cancer patients to COVID-19. Another study from Memorial Sloan Kettering Cancer Center looked at a cohort of 423 cancer patients with COVID-19 (8% of which were lung cancer patients) and found that 20% developed severe respiratory illness (including 9% who required mechanical ventilation) and 12% died within 30 days. In addition, the authors found that administration of immunotherapy was associated with a higher risk of complications. Despite small sample size of patients from single institutions and from different countries, all these studies reinforce two points: cancer patients may be at a higher risk of developing complications from COVID-19 and various patient- (such as lung damage from radiation therapy) and treatment-specific (immunosuppressive treatments such as chemotherapy) factors determine the extent of severity.
- New research out of China suggests that the antibody response (a measure of immunity) to SARS-CoV-2 infection may not last as long as for other respiratory viruses, particularly among asymptomatic patients. The study, published in Nature Medicine, suggests that antibody levels fall off by over by 70% in both asymptomatic and symptomatic patients by 8 weeks following infection. Though the sample size is small, if true, these results have important implications for establishing “herd immunity” (also sometimes referred to as community immunity) through natural infection as well as vaccination efforts.
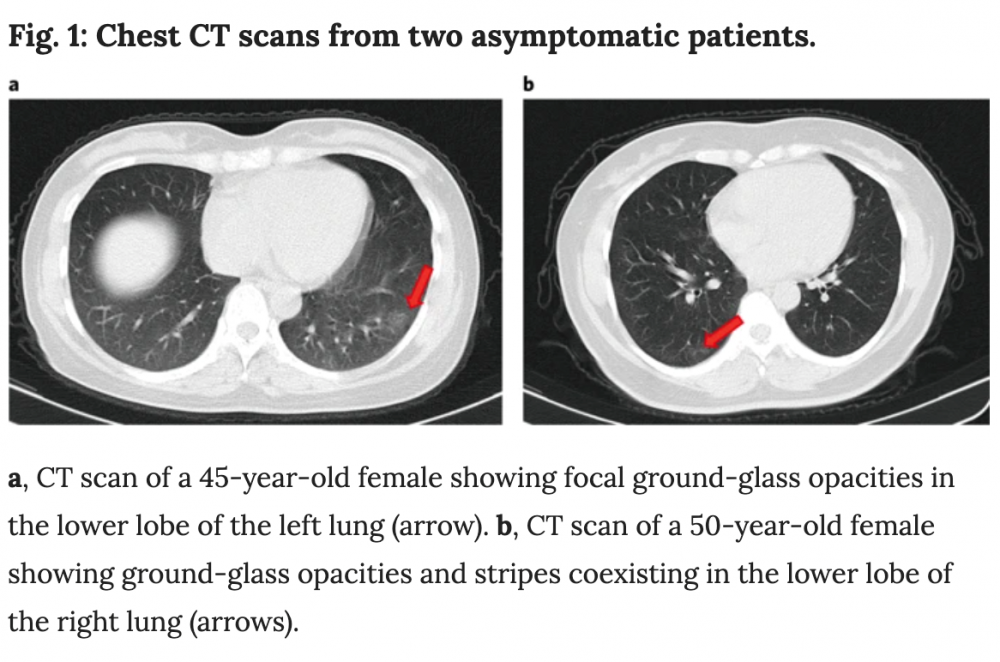
- Additionally, the paper above described radiological imaging findings in the lungs of asymptomatic patients, including ground-glass opacities as shown below. Coupled with prior reports of extreme lung damage in some patients (including a healthy 20 year old woman who required a double-lung transplant), these data, though from a small cohort of patients, affirm that there is still much we do not know yet about COVID-19’s impacts and if infection has a lasting impact on lung function in patients who recover. In the case of lung cancer, the overlap between radiological findings in COVID-19 and lung cancer complicates diagnosis, treatment and management of patients.
In light of these studies and others which suggest an increased risk for patients with lung cancer, researchers from the fields of lung cancer, virology, immunology and epidemiology are rapidly mobilizing to create large-scale programs to address questions such as:
- What is the relative risk of COVID-19 for lung cancer patients?
- How many lung cancer patients have been infected with SARS-CoV-2 and have antibodies against the virus?
- What are the features of the immune response to SARS-CoV-2?
- What are the long-term implications for lung cancer patients who recover from COVID-19?
In summary, we continue to advise our community to maintain public health precautions as they go about their daily activities such as household chores and groceries. In a recent New York Times article, former director of CDC (under the Obama administration), Dr. Tom Frieden says, “Start with the three Ws: wear a mask, wash your hands, and watch your distance.” Now more than three months into the pandemic, hospitals and clinics have excellent procedures in place to ensure that patients are kept safe during clinic appointments. We strongly advise lung cancer patients to check with their doctors on what these precautions are, in case they are concerned about getting exposed to SARS-CoV-2 while seeking healthcare. It is not advisable to miss clinic appointments without consulting your healthcare team.
AACR Virtual Conferences
Lung cancer patient advocates attended AACR’s Virtual Annual Meeting II on June 22-24. As expected, many presentations focused on the intersection of COVID-19 and cancer as well as our current national dialog on racial issues. Dr. Lisa Newman presented work on the double hit minority cancer patients are facing as a result of the ongoing pandemic. Dr. Ned Sharpless, Director of the National Cancer Institute (NCI), reported data predicting an additional 10K cancer deaths over the next decade as a result of missed screenings, delays in diagnosis and reductions in cancer care. Though these models were for breast and colorectal cancer, there is equal concern about the potential impacts on lung cancer. The lung cancer advocacy groups must continue to push forward policies that protect minority communities and ensure access to continued screening and care during the current crisis.
Thank you to everyone who participated in our recent survey to collect data on the value of these updates and patient concerns that have emerged as a result. We are pleased to report that we have had two abstracts accepted for presentation at the upcoming AACR Virtual Meeting: COVID-19 and Cancer being held July 22-24. Our community will be well-represented as we learn even more about the intersection of these two diseases and the implications for lung cancer in particular.
Resources and websites:
- IASLC’s Guide to COVID-19 and Lung Cancer
- The National Cancer Institute has a special website for COVID-19 and emergency preparedness. COVID-19: What People with Cancer Should Know-
- We are following updates provided by the World Health Organization (WHO) and the US Centers for Disease Control and Prevention (CDC)
- Johns Hopkins COVID-19 Resource Center
- Interactive map of US COVID-19 cases by state
- The One-Two Punch: Cancer And COVID-19 (an important perspective for cancer patients)
- You can find information specific to your state or city or town on your health department’s website.
- American Medical Association resources for healthcare providers.



GO2 for Lung Cancer (Amy Moore, PhD – amoore@go2.org)
LUNGevity Foundation (Upal Basu Roy, PhD, MPH – ubasuroy@lungevity.org)
Lung Cancer Foundation of America (Kim Norris – KNorris@lcfamerica.org)
Lung Cancer Research Foundation (Jan Baranski, PhD – jbaranski@lcrf.org)
LungCAN (Kimberly Lester – kimberly@lungcan.org)

Leave A Comment