As of July 1, 2020, more than 10 million people worldwide have been infected with SARS-CoV-2, the virus that causes COVID-19. In the United States alone, more than 3 million people have tested positive, as of July 10, 2020. Our knowledge about how the virus affects our immune systems and other organs is continuously evolving. Along with this knowledge, doctors are becoming better at managing patients with a confirmed diagnosis of COVID-19. However, it is important to keep in mind that the virus is still infectious.
In this update, we answer some key questions about the current need for public health measures, testing in light of the recent rise in COVID-19 cases, what the test results means, some recent press on “new strains” of SARS-CoV-2, and finally what this means for herd (community) immunity.
What public health measures can help stop the spread of the virus?
Current data still suggest the virus is most commonly spread person-to-person, via droplets expelled by talking, coughing, or sneezing while in close face-to-face contact. The virus may also spread via aerosols (smaller droplets that remain suspended in air) but at this point, this has not been clearly established. People can have an active case of the virus and show no symptoms (asymptomatic spread). Until a vaccine is available, we need to take action to prevent transmission of SARS-CoV-2 through these strategies:
- Personal hygiene (e.g., hand washing)
- Testing people to identify cases of active infection
- Using distance or physical barriers to reduce the spread of infectious droplets (e.g., staying home, social distancing, wearing masks, isolating people who are infected)
- Contact tracing (e.g., notifying people when they have been in contact with someone who has active infection)
- Government-level actions (e.g., governmental limits on sizes of gatherings or business capacity; school or workplace closures; stay-at-home orders)
- Travel restrictions (e.g., border closure, enforced quarantine on visitors from infected areas) if required
Should I get tested for COVID-19? Which test is right for me? What do the test results mean?
If you or your loved one suspects that they have been exposed to SARS-CoV-2, and/or have developed the three most common COVID-19 symptoms (fever, cough, and shortness of breath), we recommend you get tested.
Currently, three tests are available for COVID-19. The choice of test depends on whether you suspect that you have an active (existing) infection, or you were infected in the past and want to confirm infection.
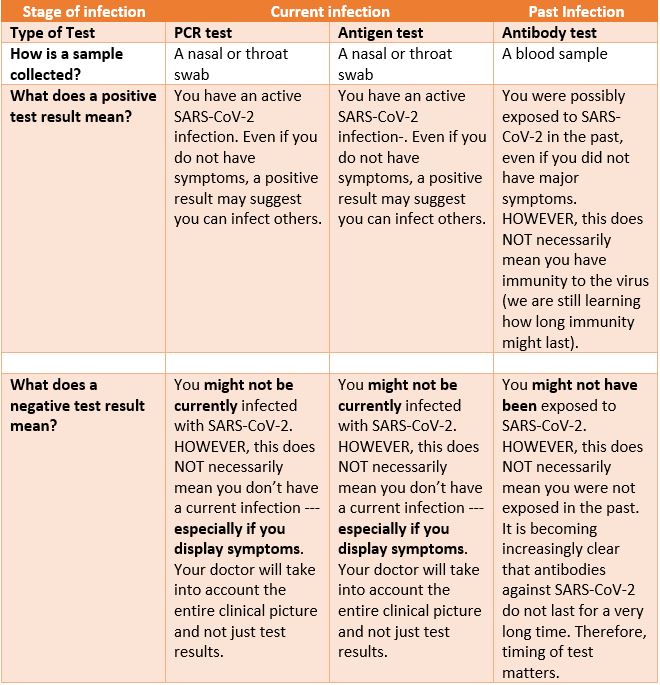
More testing will help us to identify more people who have an active case of COVID-19 and may be able to spread the disease, whether or not they have active symptoms. An accurate count of active cases tells us where the virus is currently spreading and hopefully helps us to implement prevention measures in time to limit spread of the disease in that area.
Has the SAR-CoV-2 virus mutated? Is this new mutation more infectious? What does this mean for prevention, vaccines, and treatment?
A preliminary manuscript (which has not yet undergone peer review) describes the emergence of a new mutation seen in a specific gene of the SARS-CoV-2 virus. This mutation, which was first discovered in Europe, is called D614G. It causes an increase in the number of spike proteins in the virus. Since the spike protein is how the virus attaches to human cells, the authors concluded that this mutation makes the virus more infectious. However, it does not appear to make the resulting disease more severe or deadly. Currently, the real-world implications of this mutation and its impact on the development of vaccines and treatments are still unclear.
Are blood tests detecting coronavirus antibodies more frequently?
Many countries are using blood tests to look for SARS-CoV-2 antibodies in their populations. Testing of blood serum is called serology. The percentage of individuals in a population that have these antibodies in their blood serum is called seroprevalence. As COVID-19 spreads across the globe, different areas will have different levels of seroprevalence.
The CDC is now conducting large-scale geographic seroprevalence surveys at a number of sites across the country. Initial results from the first six sites showed rates of people who tested positive for SARS-CoV-2 antibodies varied from about 1% (in WA state) to about 7% (in greater NYC area).
Several global seroprevalence studies have been published recently. In Spain, which was hit hard by COVID-19 in the spring of 2020, approximately 5% of people in the 36,000 households tested had antibodies against SARS-CoV-2 (they are “seropositive”—their serum tested positive for antibodies). The seropositive rate is closer to 10% near Madrid but only 3% along the coast. Given that 95% of Spaniards do not have antibodies (seronegative), the authors conclude that it is important to maintain the public health measures described above.
A second study from Brazil also found regional variability in seroprevalence, with an overall seropositive rate of 1.4%. However, surprisingly, some cities along the Amazon had some of the highest rates reported so far, approaching 25%. This finding further counters the argument that SARS-CoV-2 is susceptible to heat, since Brazil maintains a hot, tropical climate.
What about herd immunity?
Herd immunity (or community immunity) occurs when a high percentage of the community is immune to a disease through vaccination and/or prior illness. We currently face several challenges to achieving herd immunity. First, seropositivity rates remain significantly below the ~70% required to achieve herd immunity, even in hotspot areas such as NYC. Second, a growing number of reports suggest that antibody levels fall off significantly as early as 8 weeks after infection (though other features of the immune system may provide some protection).
Some have suggested that public health efforts to reduce transmission are only delaying the acquisition of herd immunity. Sweden has been held up as a model for keeping a country open to develop herd immunity. However, Sweden serves more as a cautionary tale— it experienced much higher death rates than its Scandinavian neighbors yet was not spared the economic impact of the pandemic. Various models have suggested that efforts to achieve herd immunity by natural infection (ie, letting the virus run its course without vaccines) would result in over 30 million deaths globally.
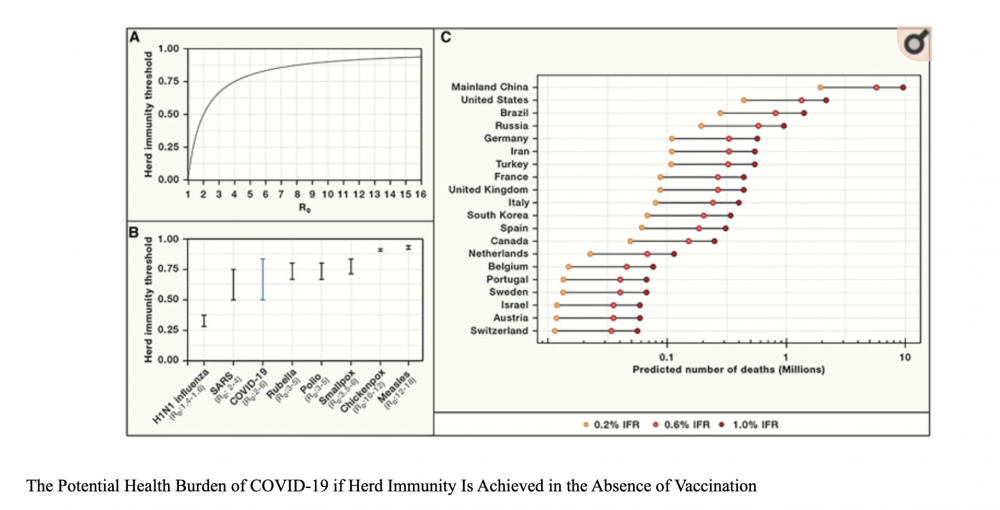
Letting the virus run its course comes at extraordinary cost in terms of human lives. Further, given the low rates of seropositivity among areas hard-hit by the virus and the rapidly declining antibody levels in individuals, it seems unlikely that we will achieve herd immunity WITHOUT a vaccine.
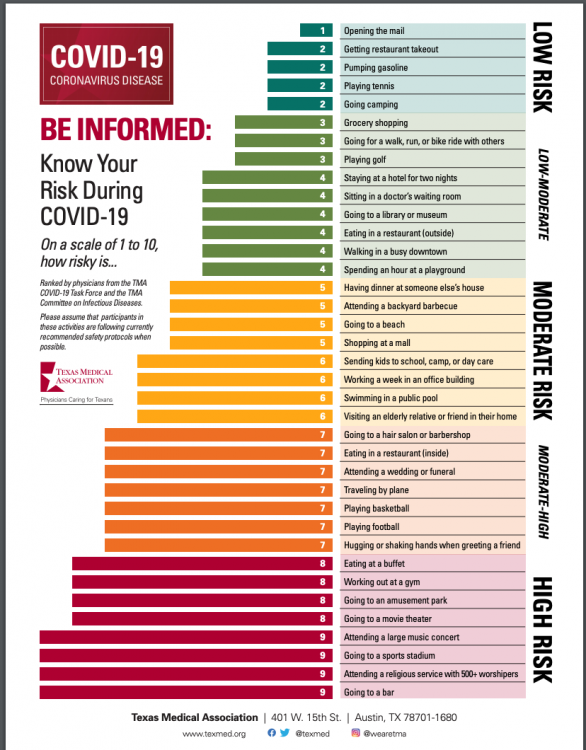
How risky is returning to “normal” activities?
These updates are intended to give you the latest evidence on what we know and to provide a framework for you to make your own decisions as we all learn how to navigate this new “normal.” In that spirit, we share this recent graphic that helps assess the relative risk of various daily activities:
Resources and websites:
- IASLC’s Guide to COVID-19 and Lung Cancer
- We are following updates provided by the World Health Organization (WHO) and the US Centers for Disease Control and Prevention (CDC)
- Johns Hopkins COVID-19 Resource Center
- Interactive map of US COVID-19 cases by state
- The One-Two Punch: Cancer And COVID-19 (an important perspective for cancer patients)
- You can find information specific to your state or city or town on your health department’s website.
- American Medical Association resources for healthcare providers.



GO2 for Lung Cancer (Amy Moore, PhD – amoore@go2.org)
LUNGevity Foundation (Upal Basu Roy, PhD, MPH – ubasuroy@lungevity.org)
Lung Cancer Foundation of America (Kim Norris – KNorris@lcfamerica.org)
Lung Cancer Research Foundation (Jan Baranski, PhD – jbaranski@lcrf.org)
LungCAN (Kimberly Lester – kimberly@lungcan.org)

Leave A Comment