Betty and Bill M. live in Castle Rock, CO where they relocated from Massachusetts in November of 2016 as part of Bill taking a new position with Boeing. They have been married for 28 years, are both native Minnesotans, and have 1 son who, after being discharged from the Marines, now lives in La Jolla, CA. After Betty’s stage 4 (IV) diagnosis she started making and selling greeting cards for which proceeds are donated to the University of Colorado Cancer Center’s Lung Fund for research. When not traveling to see family around the country they enjoy going out to movies, are close to their “small group” from their church, socialize with friends, and chase after their dogs Jazzy and Bailey.
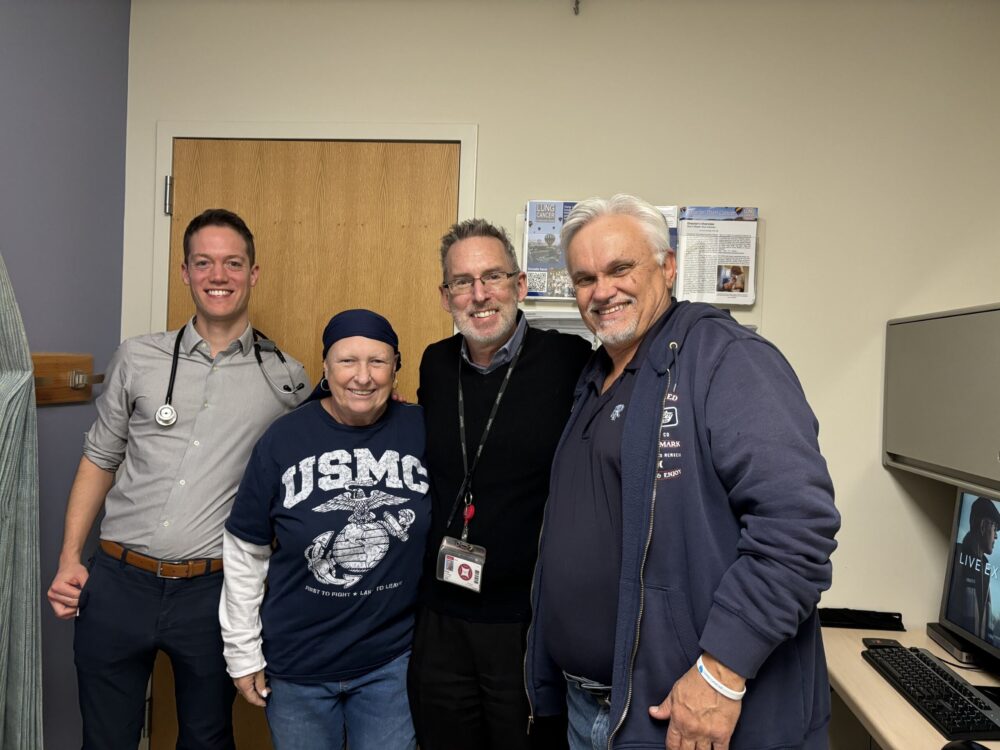
Since Betty’s diagnosis with lung cancer in the spring of 2017, she has endured over 1,000 different tests, had 100+ scans, gone to the ED 20 times, was admitted 10 times, and met with her care team over 200 times for procedures, infusions, office and clinic visits. Bill was by her side for every single one.
“Our” diagnosis
Betty: A little over 7 years ago, I started having spasms in my back. That was a new thing for me; they were very painful and kind of scary. Eventually, those spasms brought me to the emergency room, where they did a CT scan, thinking I had a pulmonary embolism.
Bill: And that’s when we found the mass. We were shocked. The spasms had actually subsided when we were in the ER, so we were anticipating the doctor to come back and say, “You’re fine; go home.” So, when he instead said, “I’m afraid we’re going to have to admit you,” we all just kind of laughed at first. He told us that they found a mass on the CT scan. And, of course, your heart just sinks.

Betty: We couldn’t believe it.
Bill: Your mind goes right to lung cancer, so it’s crushing. We were admitted for a night or 2 and then sent to a specialist to do a biopsy using an endobronchial ultrasound (EBUS) procedure. That took a few weeks to get lined up, so we were living for a month with this uncertainty and clinging to hope that it was one of the other things they said it could be.
Betty: The timing was especially terrible because our son, our 1 and only child, was about to leave for boot camp to become a Marine. That was heavy on our minds, and scary for him, too. He even considered not going because we didn’t know what would happen with me while he was gone, but we told him to go.
Bill: When our results came in, some random doctor sat down with us and said, “Unfortunately, I’m here to tell you that you’ve got lung cancer.” I’ll never forget it; it was so harsh. We both said, “Well, what do we do next?” And she just said, “Well, you need to find an oncologist.” That was the end of the appointment. That’s all she told us. She gave us the news and sent us on our way without any other guidance. We went home and cried a lot.
Betty: I didn’t cry.
Bill: (laughs) Well, I did.
Betty: The only thing I heard from the doctor was the word “unfortunately,” and then I shut down. I have no idea what she said after that. But I think I was the person who said, “So, what’s next?” I’m not very good at waiting. I just wanted to get going.
Bill: We wanted to get going because what else were we going to do? We wanted to get to it.
Betty: I want to make sure to point out that from day 1, from that very first drive home, I have never, ever heard Bill say, “Betty’s cancer” or “Betty’s treatment.” It has always been “our cancer, our doctor, our treatment.” Bill is so kind; I’ve always known that about him. But I didn’t know he would take on my cancer as his cancer, as our cancer. It makes me feel taken care of.
Bill: I never even thought about it, but I do feel like it’s our disease and our diagnosis. The cancer is in Betty physically, but it’s our family’s cancer. It’s all of ours.
Starting treatment: “The longer you live, the longer you’re going to live.”
Bill: Our first oncologist at the University of Colorado Cancer Center wasn’t the right fit for us. He didn’t have a very good bedside manner. He bluntly told us that Betty had 6-9 months to live. But Betty and I had different opinions on what to do about it. I believed that it didn’t matter that he wasn’t the most personable, we just needed someone who was medically competent, which he was. He made the right initial treatment decision for us, which was 2 chemotherapy treatments, Paraplatin (carboplatin) and Alimta (pemetrexed), as our standard of care.
Betty: But I read a book that said, “If you can’t hug your oncologist, you should get a new oncologist.” We definitely couldn’t hug this one. So, I told Bill that I just didn’t have a good feeling. He wasn’t happy to have to make a change already, but I’m glad he listened to me.
Bill: At the end of the day, even though we look at it as our doctor, technically, it’s Betty’s doctor. It was her decision.
Betty: I told the nurses I needed a new oncologist and asked if they knew a good one. They recommended Dr. Regina Brown and I got to meet her that day.
Bill: Thank God Betty stuck to her guns because Dr. Brown is an angel. I get choked up talking about her. She really saved our souls along with taking care of the cancer. She didn’t change the treatment the first doctor gave us, but she was what we needed in every other way. She has a big personality. She hugged us every time we saw her and cared about us as people. She’d ask about our family, our life, and our son. She’d always say, “How’s the Marine doing?” She helped us to emotionally navigate the diagnosis. That was really what we needed.
Betty: I’m still mad at her, though.
Bill: (laughs) Because she left?
Betty: Because she left.
Bill: When she told us she was leaving the practice, it was nearly as devastating as getting the diagnosis to begin with. It was a gut punch to both of us.
Betty: This time, I did cry. All 3 of us did.
Bill: But before that, Dr. Brown was with us through COVID, and she helped us through the side effects Betty got from Paraplatin (carboplatin) and Alimta (pemetrexed). Carboplatin is tough stuff. It’s good stuff. It works. But it’s brutal. We had a couple of hospitalizations for neutropenic fevers. Betty had one in particular that was really, really bad. She set the hospital record for her fever – 106.7 degrees. It is not a record you want to own.
Betty: Well, I was kind of proud actually.
Bill: Go big or go home.
Betty: (laughs) That’s what I did. I went big.
Bill: Well, she went big almost to a bad ending. It was scary. Betty then went on Alimta (pemetrexed) as maintenance chemo. It seemed to be working but it also started to cause kidney damage. So, Dr. Brown then put us on Opdivo (nivolumab).
Betty: It had just been FDA approved for lung cancer.
Bill: Dr. Brown told us at the very beginning that this is a great time to have lung cancer. And she said something that has stuck with me since then: “The longer you live, the longer you’re going to live.”
Betty: They’re words we live by.
Bill: Opdivo (nivolumab) wasn’t a choice when we first started the chemo, but then it was approved, and it worked for us for two years. It was so much more tolerable. Also, we only had to go once a month for the Opdivo (nivolumab) infusion, so our quality of life improved because we had fewer appointments.
Read part 2 of Betty and Bill’s story.

Great story! Great couple! Thanks for sharing!
Where is part 2?
Hi Aimee! Part 2 is coming out in our September 12th issue of Your Community!