GO2 for Lung Cancer’s recently published scientific paper found that lung cancer screening programs can successfully detect lung cancer early with the majority of lung cancers diagnosed at stage 1 or limited stage. Importantly, outcomes at academic and nonacademic sites were compared and the data confirmed that responsible screening can take place in a community setting.
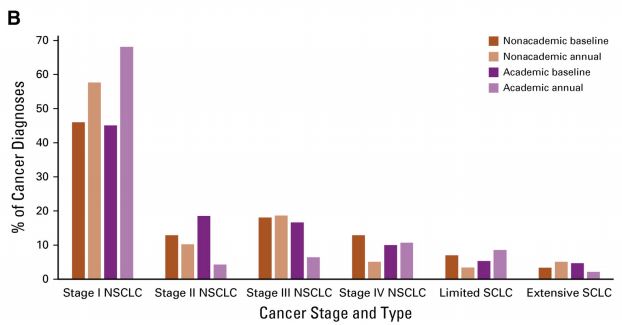
Figure B: Percentage of each stage and type of lung cancer diagnosed at nonacademic centers compared with academic centers.
Published in the respected Journal of Oncology Practice, the paper resulted from data collection from our Screening Centers of Excellence (SCOE) network. This is one of the first publications assessing workflow, outcomes, and barriers at community-based lung cancer screening sites.
Our team analyzed survey data from our SCOE network of over 600 lung cancer screening programs committed to following best practice protocols during the first year of insurance coverage for lung cancer screening. The paper shares important information about an effective screening program framework that others may use to evaluate and improve their programs.
While this data validates our SCOE network as a fundamental tool in defining high-quality and effective lung cancer screening, screening is still a relatively new practice which faces barriers. More than 50% of screening program representatives in the study reported that insurance and billing issues, lack of patient awareness about screening availability, internal workflow issues, and problems with provider referrals were barriers for their program. These findings highlight the immense value of our SCOE network, while also underlining the opportunity to address barriers and increase the impact of screening for our community.
Congratulations to our science and research and excellence in screening and care teams for this major accomplishment.
You can access the full publication for free! Click here to view or download.

When will screening be recommended for those of us with family history? Both my mother and father AND maternal grandmother died of lung cancer and yet I am not eligible for screening. Seems like a no-brainer to me, but yet I am denied access to screening. Are we still waiting on family history to be proven as a risk factor?
Hello Carol,
I’m so sorry to hear of all the losses you have had because of lung cancer. We understand your concern and we are working to better understand to what degree family history is a risk factor.
As an organization, we know current and former smokers do not represent the totality of those diagnosed with lung cancer. We have conducted awareness campaigns around lung cancer in never smokers and include this information in all of our fact sheets. Many of our volunteers and advocates are younger people, and most recently, young women, who never smoked are increasingly being diagnosed.
Current screening guidelines are were established based on the results of the large National Lung Screening Trial (NLST) a few years ago that showed screening people at known high risk (smoking history) for lung cancer can reduce mortality from the disease by at least 20%. When setting guidelines for screening, there needs to be a body of supportive evidence which shows that the benefits of screening outweighs the risks (such as radiation exposure in the case of lung cancer screening). While screening for lung cancer uses lower doses of radiation compared to a regular CT scan, it is still considered to be a greater risk than benefit until we can better understanding risk factors (including family history).
Currently, we don’t have a way to identify people at risk who are outside current screening guidelines; but we are action-oriented and particularly dedicated to more fully understanding why more young, never smoking women are being diagnosed with lung cancer. GO2 for Lung Cancer played a critical role in crafting the 2018 and 2019 Women and Lung Cancer Research and Preventative Services Act (https://lungcanceralliance.org/advocacy/our-legislative-priorities/women-and-lung-cancer-research-and-preventive-services-act/) and passionately appeal to federal legislators to pass the Act by asking our community and the public, to take action (https://lungcanceralliance.org/advocacy/our-legislative-priorities/women-and-lung-cancer-research-and-preventive-services-act/) by contacting their representatives and by going to Capitol Hill during the National Advocacy Summit to ask legislators to sign onto and ultimately pass the Act. We have had legislative successes in the past and are committed to this effort.
We also continue to look for ways to partner and support ongoing research efforts to better understand who, precisely, is at risk for lung cancer and to develop new screening methods that will work to identify lung cancer in those outside current screening guidelines. The Lung Cancer Registry is just one way we are trying to understand risk and treatment options better. You can also see a study being done through Dana Farber by clicking here (https://www.dana-farber.org/thoracic-lung-cancer-treatment-center/inherited-egfr-t790m-mutations/).
Please feel free to reach out by phone or email, if you have additional questions. If you are interested in helping us advocate for expanding screening, the hyperlinks in this post to learn about ways to advocate with us.