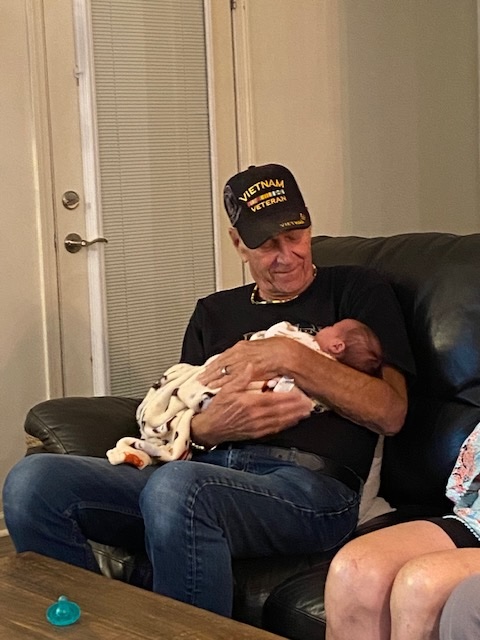
Jim Fackler lives in Lancaster, South Carolina, with his wife, Gail. He is a proud Vietnam veteran who served in the United States Navy. He enjoys golf, driving his pontoon on the lake, home improvement projects, and meeting with other veterans. Jim and his wife also love to travel and are planning a trip to Amsterdam and Belgium this summer.
In September 2021, I was told I had stage 4 (IV) small cell lung cancer (SCLC). To say I was in shock doesn’t even begin to describe what I felt when I was given the news. After the initial diagnosis, further testing found that the cancer had spread to my hips, abdomen, and brain. Today, 2.5 years after my diagnosis, I’m very happy to say that the cancer appears to be gone from my brain, hips, and abdomen, with only a small node left in the lung.
My diagnosis
In July 2021, I started coughing and assumed it was just a summer cold. As time went on and the cough persisted and started affecting my sleep, I got in touch with my Veterans Administration (VA) doctor. We were still at the height of COVID-19, and the VA was not seeing patients in person, so we communicated via email. They thought my blood pressure medicine was the problem, so we changed medicines. When that didn’t work, they thought I had asthma and sent me an inhaler.
At that point, because the coughing was getting more persistent, my wife felt it was time to find a private doctor to see me. As soon as my doctor heard my cough and listened to my lungs, he said he wanted to get a CT scan done. I will never forget the day I went in for the results. I had the CT scan on Sept. 1, and on Sept. 2, I was given the news I hoped I would never hear. It was apparent the minute the doctor walked into the exam room that the news was not going to be good. He said, “I’m sorry to tell you that you have stage 4 (IV) lung cancer.”
I’m not sure what adjectives best describe what I felt at that moment, but disbelief and numbness are the first things that come to mind. Feeling like my world just came to an end and feeling scared and hopeless were just the beginning of a long string of emotions. I wasn’t sure how I was going to tell my wife.
After being referred to an oncologist and going through a lot of tests to determine the extent of the cancer, my healthcare team sent me to a pulmonologist for some additional tests. He provided the first glimmer of hope when he told me that treatments have come a long way in the past few years. He told me that if I had received this diagnosis even 5 years earlier, I probably would not have long to live, but he felt optimistic that I had some good options with treatments that are available today.
Turns out he was right.
Being a veteran with SCLC
If the VA had a process in place for annual CT scans of every veteran who served in Vietnam, they might have been able to catch my cancer at stage 1 (I) or stage 2 (II), and it might have been curable. For me, exposure to Agent Orange and having a history of smoking (even though I quit 25 years ago) increased my risk of developing lung cancer. Unfortunately, 50 years ago, no one knew that exposure to Agent Orange and cigarettes could cause cancer.
I hope that sharing my story as a Vietnam Veteran with SCLC will impact members of Congress and the Senate who control lung cancer research funding. I want to impress upon them how important additional federal funding is to finding cures for this devastating disease and saving lives. My message for Congress and the Senate is: “I fought for my country; now I am asking my country to fight for me, other veterans, and lung cancer survivors.” We need to continue to find out why SCLC metastasizes (spreads) the way it does so that new drugs can be developed to combat the spreading of cancer cells throughout the body without the harsh side effects.
Living with lung cancer
Living with lung cancer has changed my life significantly. Both my wife and I have had to learn to live one day at a time because I do not know what tomorrow will be like for me.
There is good news in all of this, though. My oncologist told me about a clinical trial in which he thought I would do well. Because I put a lot of trust in my oncologist, I agreed to participate in the program. After going through chemotherapy and radiation, I now go to the cancer institute every 3 weeks for an immunotherapy infusion. This has helped to keep the cancer at bay for now and has given me a longer life than the expected range for my diagnosis. I strongly believe that I am still here today because of the clinical trial drug I receive with these infusions.
However, the cancer treatments I receive have come with side effects. I have lost my balance and am no longer stable on my feet. My speech has become slurred, making it difficult for me to communicate clearly. My appetite and energy are also affected but are minor, next to my speech and balance issues. I’ve lost more than 60 pounds since my diagnosis—not a weight loss plan I would recommend for anyone.
Because of my treatment schedule, I live my life 3 weeks at a time. Plans for activities and vacations are scheduled around and must fit within the confines of my treatment plan. However, I am still staying active, traveling, and staying involved with lung cancer groups. Last year, my wife and I went to Switzerland for 3 weeks during the summer and then to the Christmas markets in Germany in December. This year, we already have travel plans for the summer and fall. You can live a good life with SCLC—you just have to plan a little differently and expect the unexpected.
Living with lung cancer is difficult, but I’m very grateful I’m still here, and I’m thankful for my treatment. I’m not going to stop living my life because I have cancer. I am going to continue to fight every day and make it difficult for cancer to live with me.
Advice for others with the disease
- Get lung cancer screenings! I want people to know that lung cancer is the leading cause of death among cancers diagnosed today. It is curable if caught early enough. If you have a smoking history, get a cancer screening yearly, just like women do with mammograms. It is easy to do and only takes minutes. You go into a tube for less than 2 minutes, and you don’t even have to take your clothes off. Results are immediate and insurance covers the cost if you meet the criteria. Annual screenings equal early detection; early detection equals finding cancer earlier and being cured so you can live a long life. One of the messages I bring back to my veterans group is: “You guys must get screened! It is essential because you have been exposed to toxic chemicals.”
- Connect with others. Being around other lung cancer survivors gives you hope, especially when you find people who were diagnosed with lung cancer many years ago and are still here today to tell their stories. It’s very inspiring. I met many people through the LiveLung SCLC group and at the GO2 Voices Summit. The people and organizations in the lung cancer community are absolutely fantastic. Those who run the organization, along with the members, are the kind of people you need to surround yourself with to know that you are not alone. They are there to help you through difficult times and understand what you are going through. They are your lifeline.
- Advocate. Being at the GO2 Voices Summit this year was worth every minute. All the time and effort people put into raising awareness and advocating for additional funding for lung cancer research makes me proud to be a very, very small part of the GO2 community. I plan to attend GO2’s Voices Summit again next year. I will continue advocating and spreading the word about getting screened early, getting involved with other lung cancer survivors, and joining an organization like GO2 that gives encouragement and hope. Having hope is so very important. It reminds you that you are not alone and that there are many people out there researching and advocating for treatments and cures for you.
If you are living with SCLC, or know someone who is, explore our special library of SCLC resources.









Jim, thanks for sharing your story! As a fellow SCLC survivor, I applaud your advocacy and involvement.
Very inspiring story!!