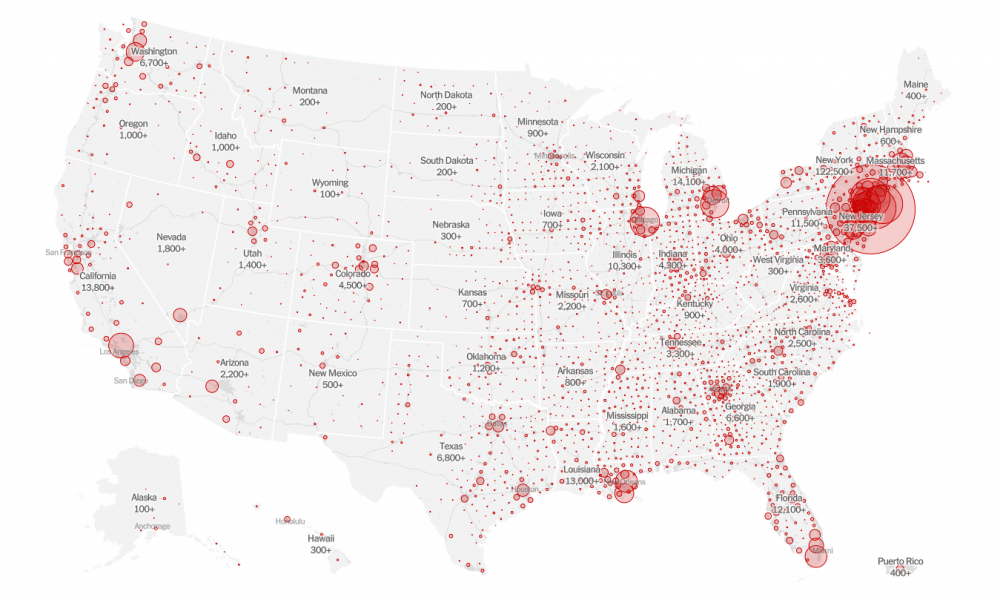
The number of confirmed cases of COVID-19 continues to grow in the US. As of April 5, 2020, there are 312,089 confirmed cases of COVID-19 in the US. These numbers may be an underestimation of the true burden of the disease due to lack of testing and a high proportion of asymptomatic yet infectious individuals.
To get a real-time understanding of the cases in the US, you can access the map through The New York Times.
In this week’s update, we answer the following important questions:
- Is social distancing working?
- Do I continue to social distance?
- Do I leave my city to go to someplace safe — such as a rural area?
- Should I use homemade masks to protect myself?
- Can I travel within the United States?
1. Is social distancing working?
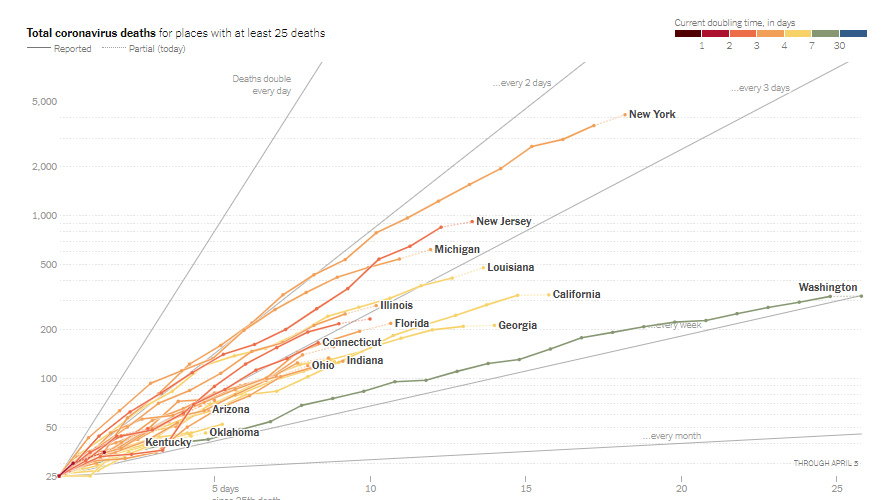
YES, IT IS! Washington and California quickly imposed state-wide social distancing through stringent shelter-in-place or Stay at Home policies once deaths occurred within their borders. The graph below shows that COVID-19 deaths are still increasing in these two states, but not as fast as in other states. Deaths in New York State are doubling every 2 days, but in Washington State deaths are doubling only every 7 days.
The most up-to-date version of the graph below can be accessed from the New York Times website here.
The CDC continues to recommend social distancing to help decrease transmission of COVID-19 within the community. Social distancing measures, such as cancelling public gatherings and avoiding crowds, can slow the spread of the virus and spread cases out over a longer period of time, which can help hospitals provide care while avoiding being overwhelmed by patients. Social distancing helps “flatten the curve” in the spread of an infectious disease.
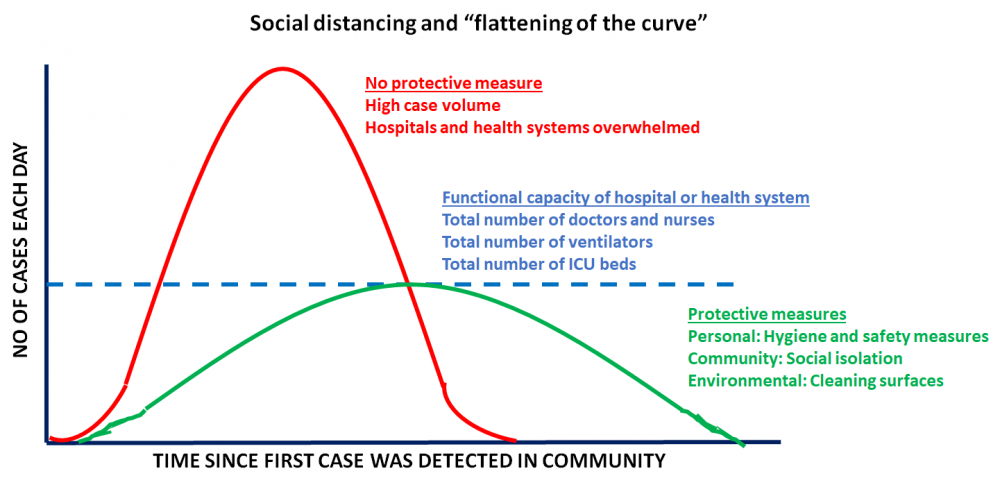
This is especially critical because hospitals and health systems are working at full capacity. Flattening the curve ensures that systems are functional and people who require care the most can get the attention they need. The CDC recommends a distance of 6 feet or 2 meters as the minimum distance between individuals as part of COVID-19 mitigation strategy.
We encourage you to check out CDC’s COVID-19 community mitigation strategies here.
2. Do I continue to social distance?
YES, social distancing is currently the only known public health measure that can protect us from SARS-CoV-2. Social distancing minimizes risk of exposure to the virus. It is important to keep in mind that social distancing is NOT the same as social isolation. We encourage you to keep in touch with all your family, friends, and loved ones through phone and video conversations. Just because we are social distancing doesn’t mean we have to be socially isolated.
Social distancing is different from self-quarantine. Self-quarantine should be practiced by people who have been exposed to SARS-CoV-2 and who are at risk for coming down with COVID-19. It involves:
- Using standard hygiene such as frequently washing your hands and not touching your face
- Not sharing things like towels and utensils with other people who share the same household
- Staying at home and not having any visitors
- Staying at least 6 feet away from other people in your household
You do not need to have symptoms of COVID-19 to self-quarantine. Caregivers who have traveled or are leaving their homes frequently to run errands may choose to self-quarantine especially in COVID-19 hot zones.
3. Do I leave my city to go to someplace safe — such as a rural area?
NO! You should not be leaving your urban apartment or home and move to a rural area for the following reasons:
- You do not know if you or a loved one has been infected with SARS-CoV-2. An infected individual might not have any symptoms but still can continue to infect others
- You may not have access to your regular doctors and healthcare in a rural setting
- Small rural areas are not equipped to handle an influx of people. They may not have adequate number of grocery and produce stores. More importantly, they may not have adequate medical care facilities should there be an emergency
Do not indulge in “disaster gentrification” for your own safety, the safety of your loved ones, and that of other community members. It is our duty to keep rural communities insulated from this disease as much as possible.
4. Should I use homemade masks to protect myself?
YES! The CDC reports that a significant portion of individuals with COVID-19 lack symptoms (“asymptomatic”) and that even those who eventually develop symptoms (“pre-symptomatic”) can transmit the virus to others before showing symptoms. This means that the virus can spread between people interacting in close proximity—for example, speaking, coughing, or sneezing—even if those people are not exhibiting symptoms. In light of this new evidence, CDC recommends wearing cloth face coverings in public settings where other social distancing measures are difficult to maintain (e.g., grocery stores and pharmacies) especially in areas of significant community-based transmission.
Masks should be worn in conjunction with maintaining adequate social distancing. It is also important to keep in mind that these face masks are not surgical masks or N95 masks (to be used primarily by healthcare works as part of personal protective equipment).
5. Should I travel within the US?
Though the CDC does not typically make suggestions about domestic travel, they highly recommend avoiding all non-essential travel within the US. Several cities and states already have a shelter-in-place order. Points to keep in mind should you need to consider domestic travel (from the CDC):
- Is COVID-19 present in your home community? If so, avoid traveling to avoid spreading the virus. You might be required to enter quarantine at your destination.
- Is COVID-19 spreading in the area where I am travelling to?
- Will you or your travel companion(s) be in close contact with others during your trip?
- Are you or your travel companion(s) more likely to get severe illness if you get COVID-19?
- Do you have a plan for taking time off from work in case you are told to stay home for 14 days for self-monitoring or if you get sick with COVID-19?
- Do you live with someone who is older or has a serious, chronic medical condition (especially important for caregivers)?
Resources and websites:
- IASLC’s Guide to COVID-19 and Lung Cancer – https://www.lungcancernews.org/iaslcs-guide-to-covid-19-and-lung-cancer/
- The National Cancer Institute has a special website for COVID-19 and emergency preparedness. COVID-19: What People with Cancer Should Know – https://www.cancer.gov/contact/emergency-preparedness/COVID-19
- We are following updates provided by the World Health Organization (WHO) and the US Centers for Disease Control and Prevention (CDC), which can be found here:
- https://www.who.int/emergencies/diseases/novel-COVID-19-2019/events-as-they-happen
- https://www.cdc.gov/COVID-19/2019-ncov/index.html
- Johns Hopkins COVID-19 Resource Center is one of the best places to get current updates. https://COVID-19.jhu.edu/
- Interactive map of US COVID-19 cases by state – https://www.politico.com/interactives/2020/COVID-19-testing-by-state-chart-of-new-cases/
- The One-Two Punch: Cancer And COVID-19 (an important perspective for cancer patients) – https://www.forbes.com/sites/miriamknoll/2020/03/20/the-one-two-punch-cancer-and-COVID-19/#73744a4358e6
- You can find information specific to your state or city or town on your health department’s website.
- A list of state department of health websites can be found here: https://www.cdc.gov/publichealthgateway/healthdirectories/healthdepartments.html
- A list of local health department websites can be found here: https://www.naccho.org/membership/lhd-directory
- The American Medical Association is also maintaining a resource website for healthcare providers. You can find more information here: https://www.ama-assn.org/delivering-care/public-health/covid-19-2019-novel-COVID-19-resource-center-physicians
- If you cannot avoid air travel, check out this handy article on “Dirtiest Places on Airplanes: How to Avoid Germs” https://time.com/4877041/dirtiest-places-on-airplanes/



GO2 for Lung Cancer (Amy Moore, PhD – amoore@go2.org)
LUNGevity Foundation (Upal Basu Roy, PhD, MPH – ubasuroy@lungevity.org)
Lung Cancer Foundation of America (Kim Norris – KNorris@lcfamerica.org)
Lung Cancer Research Foundation (Jan Baranski, PhD – jbaranski@lcrf.org)
LungCAN (Kimberly Lester – kimberly@lungcan.org)

Leave A Comment